For our HLSA friends in the South Texas Chapter of HIMSS, there will be an AI Summit on Leveraging AI in Healthcare at the Chapman Center of the Trinity University Campus on May 2, 2024. Discover how AI is being used to enhance patient outcomes, streamline processes, and improve overall healthcare delivery. Network with professionals and gain insights into the future of healthcare technology. Don’t miss this opportunity to learn about the latest advancements in AI and its impact on patient care! See the agenda and times below. Seating is limited and going fast so register now!
AI Summit: Leveraging AI for Healthcare
Date: May 2, 2024
Location: Trinity University; Chapman Hall & Great Hall
Agenda:
3:00pm- 3:30pm- Check-In
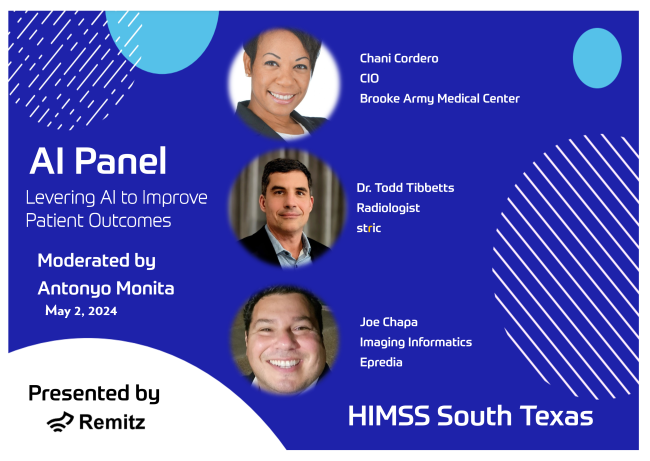
3:30pm-4:30pm – AI Panel Discussion
4:30pm-5:00pm – Q&A
5:00pm-7:00pm – Networking Social
Join us at the AI Summit where experts in the field will discuss how Artificial Intelligence (AI) is revolutionizing healthcare.